Lessons in Resilience: A New Safety-Focused Bed Tower Adapts to the Pandemic

The 7-story Sharp Chula Vista Ocean View Tower opened on January 14, 2020, just a few days after the World Health Organization issued an alert that a new coronavirus had appeared in China. By January 21, the Centers for Disease Control had confirmed the first case in the United States. Annie Chiang, one of the project architects who spent more than four years and 7,000 hours working on the project, wanted to understand how the new tower, planned and designed to meet High Reliability Organization (HRO) standards, adapted to the crisis so soon after opening. She recently spoke with Christine Basiliere, Vice President and Chief Nursing Officer at Sharp Chula Vista Medical Center, and Matthew Teichner, Senior Project Manager with Sharp's Facilities Management and Development department, to understand the impact that the planning layout and resources of the newly built Ocean View Tower had on Sharp’s COVID-19 response. The following excerpts from that conversation have been edited for length and clarity.
Annie Chiang (AC): The novel Coronavirus pandemic hit San Diego County at a time when Sharp Chula Vista was just occupying the new hospital tower. Within three months of the grand opening, you were pressed to make quick decisions to prepare for a health crisis at a scale no one could fully appreciate. How did the pandemic change the intended use and operation of the new tower?
Christine Basiliere: You know, without ever seeing COVID-19 coming, the tower timing could not have been more perfect. Prior to the expansion, we had become masters of throughput in the existing facilities, optimizing every single space that you could imagine, which is why we needed the additional tower. While we had the experience of running at full capacity before COVID-19, had we not had the new tower, I don't know how any of our COVID strategies would have been able to work.
Our first COVID-19 case was admitted to the Ocean View Tower (OVT) on March 13, where we had available negative pressure rooms. By May 3, we had hit our peak at 61 positive patients, and we've been averaging about 40 positive cases since the pandemic began. In these latter months, we've changed our strategy, using the new beds in the OVT to help us segregate non-COVID patients and concentrating COVID care to the existing hospital.
Matthew Teichner: Christine, one thing I would note is, especially when we were at the 61 peak, there were still probably anywhere from 14–16 PUIs (patient under investigation). So our nursing staff was really dealing with 70+ people, all cases where they were having to fully garment to care for them.
Basiliere: Back then, because testing wasn't as quick, patients remained under investigation for some time. We had ICU (intensive/critical) level of care or PC (progressive/intermediate) level of care. We segregated all patients needing aerosolizing procedures into the ICU level. And then we did droplet contact for non-aerosolizing patients at the PC level. We still needed additional negative pressure capacity, but it's very expensive to create temporary negative pressure rooms. Because we couldn’t know what our peak would be, we devised a strategy to build temporary negative pressure rooms in groups of seven each week, to align with how the virus was duplicating every six days at that point.
Our thinking was that it would keep us ahead of the need but limit expense. It was kind of a funny math, but it worked for us.
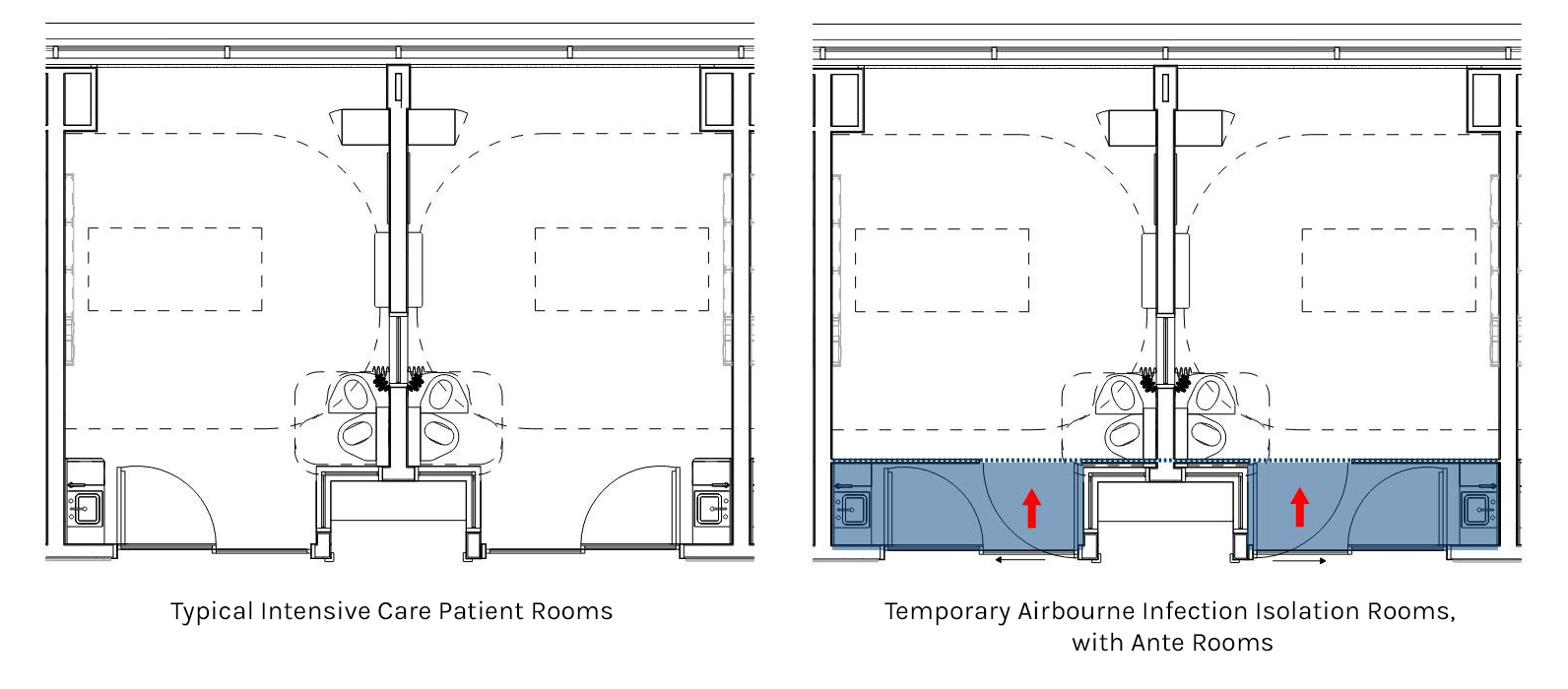
Teichner: And COVID patients’ length of stay tends to be much longer, which takes up capacity fast. We had 28 beds in the MICU (medical intensive care unit) in the existing bed tower and two already had built-in negative pressure; we installed 26 temporary negative pressure rooms there on March 16. When we filled that up, we converted the new OVT SICU (surgical intensive care unit) to nine temporary negative pressure rooms on March 23. We created another COVID PCU on a portion of the fifth floor of the existing hospital tower, where we installed two temporary ante-rooms on March 30 to essentially cordon off that unit. This was all in the space of two weeks.
Basiliere: The new OVT PACU (post-anesthesia care unit) became our non-COVID ICU, with up to 10 patients. Having that PACU, which we didn't have before the OVT, and the SICU let us segregate non-COVID from COVID patients. We were able to manage it that way, and it worked—it helped us through the peak.
I really believe the new tower was our saving grace in so many ways because we were also able to transfer and segregate patients admitted through the ED.
The way that the PACU and Pre-Op in the new tower are located together in one, integrated platform was so beneficial to repurposing that space as a temporary ICU. It was a lever that, when pulled, just let all the pressure out.
Teichner: It was a really minor conversion. We added a couple of hose bibs at some sinks so they could do dialysis, too; which it was never designed to do, but it was an easy modification and it worked perfectly.
AC: We have been helping health systems across the country find ways to create more negative pressure rooms during the pandemic, but I’m curious about what other adaptations were necessary in your facility, that perhaps could be designed in future facilities?
Basiliere: One thing we could better plan for in future facilities is visual access to the patient while operating in an infectious crisis mode. In that mode, you need the ante room outside the patient room for donning and doffing so that nurses don't have to constantly wear PPE. The problem is it doesn't give you visual access to the patient, so to check on any patient you have to get into full PPE. If the space doesn't allow for installation of windows for visual access, then perhaps we could have video monitors in the room.
[Interviewer Note: The 6th floor of the Tower was shelled for a future patient floor. Eight months after opening, five months into the pandemic, Sharp asked SmithGroup to study fit-out options far ahead of schedule. We explored both increasing the number of isolation rooms or adding typical progressive care rooms that can be converted to airborne infection isolation (AIIR) as needed. We also studied increasing the glazing from a narrow lite to a half lite in both the anteroom and the patient room door. By aligning the entry door with the toilet room wall, rather than offset, we can achieve better sightlines to the patient.]
Another thing is that the temporary HVAC systems make the environment extremely loud. Comms systems and headsets don't work under all the PPE so we saw people go back to archaic ways of communicating, like writing on windows, because they just can't hear each other. It would be great if there was a way to achieve the temporary negative pressure without the loud blowers in the future.
A lot of our other Sharp hospitals put the IV pumps outside of the patient room, to decrease nurses going in and out. We couldn’t do that at Chula Vista because of the larger rooms. It would have required more power and tubing extension than we could effectively manage. In a new build, it would be interesting to see whether we could design for the pump outside of the room for situations like these.
I think staff are willing to have smaller ante rooms than code allows. The ante rooms took up so much space that we weren't able to get pumps and other equipment outside of the room; the tubing would have been 25-plus feet.
[Interviewer Note: According to California Building Code 2019, Section 1227.12.3, an anteroom shall have at minimum a handwashing station, 3' work counter, cabinets, and space to gown and to store clean and soiled materials. This code requirement resulted in more square footage than Sharp felt was needed to perform their tasks efficiently. Sharp opted to create minimal temporary ante rooms with a depth just large enough for a door swing and gurney passage. Many of the temporary anterooms installed in existing ICU rooms have only hand-sanitizing dispensers, a PPE dispenser for gowning, a waste receptacle to dispose soiled materials, and minimal or no work counters.]
Teichner: There's a psychological element to how we’re being forced to provide care now, too. The MICU is a tough place to work normally, but our people are spending 12.5-hour shifts, all week, there. You can imagine the toll that's taking on them.
AC: Do you feel that you have enough respite areas for your staff? If not, how have you adapted to provide those spaces?
Basiliere: Because we have limited visitors now, we are using the OVT visitor lounges as additional respite spaces for the staff. We had to limit the break rooms to one or two occupants to account for social distancing, per CDPH (California Department of Public Health).
We are also using the lobby and we repurposed other public spaces for the staff. For example, we put some long tables on the new terrace outside of the chapel and opened up the meditation garden to let staff eat outside while having enough space for social distancing.
Teichner: Our 140-seat cafeteria went to 20 seats real fast. Only one or two of the food service stations are open now. Everything's pre-packaged.
Basiliere: Our rooftop café has social distancing queuing dots, and you can only sit here and there. But the outside spaces really do help people de-stress.
AC: Did you adapt or repurpose any of the back-of-house or other support spaces?
Basiliere: At some point, we looked for places where we could hang laundry line and sterilize masks and other PPE. We looked at the shelled sixth floor, where we could use the natural UV light from the windows, or a place where we could use a UV robot. We didn't end up using that strategy, but it was discussed.
We did need more scrub storage space. Normally, staff wear their scrubs in and take them home and wash them, but now people have to leave their scrubs. We also needed more showers because the staff now shower before they leave to protect their families and people on the outside. We took over patient showers for the staff.
AC: Circulation and access are such important considerations in limiting infection spread. How has circulation and the number of entry points changed?
Basiliere: We created an Excel spreadsheet of every single entrance and then we sat and figured out how to lock it down, whether it has a boundary or a key lock. I think we had 27 different entrances and exits before the pandemic, and we've now limited to four or less because they all have to be manned. Primarily for visitor control: there was a lot of confrontation with visitors in the beginning. And secondly, for controlled access for staff. Each entrance is manned by personnel who do employee screening and visitor or vendor screening.
Teichner: The main OVT entry lends itself very well to the situation, whereas the other entries to the older facilities function less well, with pinch points or poor flow. We don't think we're going to open all our doors back up, post-COVID.
AC: When you were hitting peak, how and when did you decide to transfer patients to other hospitals?
Basiliere: Because coronavirus is novel, we didn't really have a precedent to go on. But we learned that each day about three of our PCU patients would take a sudden turn and need to be moved to the ICU. If we were down to five negative pressure rooms, we knew that we could anticipate three admissions from the PCU, leaving us with two negative pressure rooms held in reserve for ED admissions. We put a protocol in place that if we were down to five or fewer negative pressure rooms that we would go on bypass. We don't like to do that because we are a border hospital, eight miles from the busiest international land border in the world.
And we're still there, we still see that same trend with COVID-19: everything's okay and then suddenly a patient just codes. That hasn't changed. That's why, in looking at designing the future patient floor, the number of negative pressure rooms will be so important.