Flexibility is the Key to Designing Health Facilities of the Future

As COVID-19 infection rates repeatedly surged across the United States, many healthcare facilities were challenged by the need to rapidly increase capacity and institute new care models and safety protocols, compounded by revenue and staffing shortages. It is more evident than ever that healthcare providers need facilities that will provide maximum flexibility to adapt more quickly in the future, whether it is to respond to changes in care delivery, technology or crises. How can we design facilities that allow for varying degrees of flexibility given the extreme complexity and uncertainty inherent in healthcare?
Emory University Hospital treated the first U.S. Ebola patients during the 2014–2016 outbreak, relying on its global leadership in infectious diseases. Recognizing that its facilities need to support the elevated protocols and treatments that Emory doctors and staff provide in these unexpected public health crises, its recent bed tower expansion integrated several new ideas that give the system a high degree of flexibility. Occupied and tested for a few years now, the concepts used in the design of the 232-bed tower may provide a prototype for designing for uncertainties like the COVID-19 pandemic.
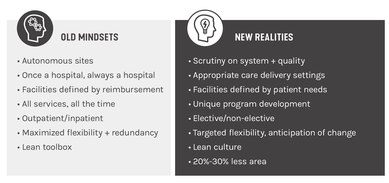
Considering flexibility from the outset, the design team for the nearly 500,000-square-foot freestanding bed tower envisioned a ‘core and shell’ hospital, without predetermined departmental locations or even any particular service lines in mind. Comparative planning that rejected traditional thinking to encompass a new set of realities led to this new concept.
The case for delaying programming decisions
In the early 2000’s, Emory University Healthcare was actively merging other hospitals into its system and changing its operational model. Growth in the system created a need for additional patient care space and expanded diagnostic and therapeutic platforms that could rapidly accommodate new technologies. Recognizing that the typically lengthy hospital construction process does not usually align with the pace of new technology, part of the premise for the core and shell approach grew out of a desire to allow for the most up-to-date concepts in healthcare delivery to be incorporated as late as possible while still allowing for a suitable construction schedule. The team dubbed this approach ‘just-in-time programming.’
Best practices in healthcare design helped to identify general requirements for very high-level programming and planning during an initial program verification stage. Conceptual and schematic design then anticipated basic essential program information, including the number of beds, the acuity of the beds, procedural platforms, support services and other non-clinical, revenue-generating services. The design team fine-tuned the building core and shell elements (structural bays, mechanical shaft locations, elevator locations, etc.) to support a wide variety of care delivery models and showed, using test fit diagrams, how the resultant plan would be able to support different models.
The programming and planning process overlaid the core and shell construction schedule so that completion of the interior design could align with timeframes for initiating fit-up construction. Working backward from construction timing to determine programming and planning targets, the project team identified more specific program and building fit-up decisions that could be made later in the schedule. While it required an added level of coordination and decision-making, these efforts afforded the project team an additional 18 months to test programming and planning scenarios, as well as to delay technology decisions to allow for the integration of the most up-to-date systems and equipment.
In the additional time afforded by the just-in-time programming, the team was able to work with doctors, nurses and staff to determine which scenarios would best serve Emory’s immediate and future needs. As the tower was constructed, it was incrementally fit up as functional decisions were made. Ultimately, the decision to approach the project this way—and the discipline to stick with it—resulted in a reduced project schedule, the most up-to-date environment, and a highly flexible chassis.
Flexible infrastructure supports adaptable programming
To establish the building’s footprint, mass and structure before detailed programming was finalized, the design team relied on site analysis, design best practices for healthcare environments, and financial considerations. As a result, floors were organized around an optimized, consistent structural grid that was more economical while still enabling a wide variety of functions and programs, including universal patient rooms, for example, which meant that either med-surg or ICUs could be accommodated as needed.
Anticipating the need for greater flexibility and adaptability in MEP systems, which may be more likely to evolve over time, the design team opted for larger floor-to-underside-of-structure dimensions of 13’-14’ minimum clear-below-structure, creating larger above-ceiling cavities throughout the tower. The larger space supports an oversized mechanical system that can allow greater air movement in infectious or high acuity situations. Larger ceiling cavities also mean better access and the ability to add or replace components with larger ones. For example, larger ducts can allow for increased airflow to higher acuity spaces and electrical/data capacity can be increased for future innovations in technology.
Two 15’-16’ floor-to-underside-of-structure floors provide even greater adaptability to unforeseen changes and developments in future care models. These taller floors can also be adapted to accommodate future research and translational functions. On-demand or speculative programs requiring more robust mechanical systems can be inserted into these two floors, allowing for the targeted flexibility health systems will need to address future uncertainties.
In addition to designing for ultimate flexibility in the new building itself, Emory opted to construct an elevated concourse system linking the tower expansion with five of its existing campus buildings. This interconnected campus increases capacity and supports adaptability on a larger scale via a system approach to care. Each building can support the needs of its patient population while also supporting secondary services and transfers from other buildings. Connected buildings can act as surge or swing space so that lower acuity patients can be relocated to appropriate environments, freeing up higher acuity space for sicker or infectious patients.

Patients, visitors and staff can easily circulate between buildings without having to go outside.
Designing for acuity adaptability can help in a crisis
Overall, the designed flexibility means that the building lends itself easily to an acuity adaptable model that can respond to a crisis or unanticipated situations—entire floors or individual units can be organized based on acuity level or disease pathway. This elasticity enables Emory University Hospital to adjust the programmatic distribution within the building and easily adapt to changing care needs now and in the future.
Today, the tower’s nursing units are organized around a disease pathway model supporting step-up acuity within each unit. Each nursing unit includes two dedicated isolation rooms for high acuity or specialty disease treatment. The antechambers of each isolation room remain positively pressurized typically but can be converted to negative pressure based on a patient’s condition. Mechanical systems are outfitted with HEPA filtration systems to serve these rooms and are designed to provide additional HEPA filtration across the entire nursing unit if needed. In addition, the building system is compartmentalized to allow for different air flows to each nursing unit separately.
Three of the tower floors are designed to support surgical platforms, D&T services or patient rooms for at-risk patients, such as cancer patients. These service lines, which usually require longer stays and a higher population of immunocompromised patients, drove some of the adopted planning and programming approaches.
The design team also recognized that, in crisis or unexpected situations, collaboration across the medical team is even more paramount. Accordingly, collaboration spaces in each nursing unit support better interdisciplinary care day-to-day while also supporting the heightened communication and collaboration necessary in a crisis.
Investing in flexibility pays off
Additional program space, interconnected buildings and higher capacity MEP systems were not without cost. All the approaches detailed in this article did come with an approximately 20% increase in first cost construction. However, the benefits they offer outweigh the initial first cost and allow Emory University Hospital to be nimble in the face of healthcare changes and as uncertainties such as pandemics arise. Deferring programmatic decisions into the construction phase enabled the design team to incorporate the most current technology and delivery practices in the most appropriate care delivery settings with the most appropriate infrastructure.
COVID-19 has been a stark reminder that the future of healthcare delivery carries many unknowns. Future healthcare facilities need to be more nimble: flexible enough to support rapid adjustments in the operational model in times of crisis and adaptable enough to support an enduring, future state health system.